Maternal mortality continues to be a serious cause for concern for pregnant women in the United States. Cardiovascular health is the leading cause of maternal mortality, according to the CDC, with the number of maternal deaths jumping by nearly 50 percent from 2020 to 2021.
Black mothers die 3-4 times more often than White mothers in the U.S., according to researchers. More than 80 percent of these deaths are preventable – even when difference such as access to health care and socioeconomic factors are taken into account. Of these preventable deaths, many are related to cardiovascular health conditions.
With these disparities in mind, Garba Rimamskep Shamaki, MD, a resident at Unity Hospital, designed a research study to examine the role age plays in these disparities and identify what age group of pregnant Black women face the highest risk of having these bad outcomes.
Explaining the study
Using data from the National Inpatient Sample Database from 2016 to 2020, the study looked at approximately 12.7 million patients who had pregnancy, delivery, and post-partum care. Of those patients, 76.7 percent were white and 23.3 percent were Black.
The patients were separated by age groups of 10-19, 20-29, 30-39, and 40-49 years. Using statistical models to determine how likely each age group would be to have certain health conditions, researchers then focused on two main groups of outcomes for each age group.
First, researchers analyzed in-hospital maternal mortality and cardiovascular outcomes for each age group. Second, researchers looked at pregnancy-related outcomes for each age group, such as preeclampsia, preterm labor, spontaneous abortion and postpartum depression.
Based on these results, the study found Black women ages 20-29 are more likely to experience higher mortality and poorer cardiovascular and pregnancy-related outcomes, even after accounting for their socioeconomic conditions and other pre-existing illnesses. Rates of hypertension, obesity, diabetes mellitus, and chronic kidney disease are significantly higher in pregnant Black women compared to white women; these differences begin in early adolescence.
What the results could mean
Traditionally, while most people in their 20s are seen as healthy and vibrant – and thus not at risk for significant health conditions or complications, this may not be the case for pregnant Black women.
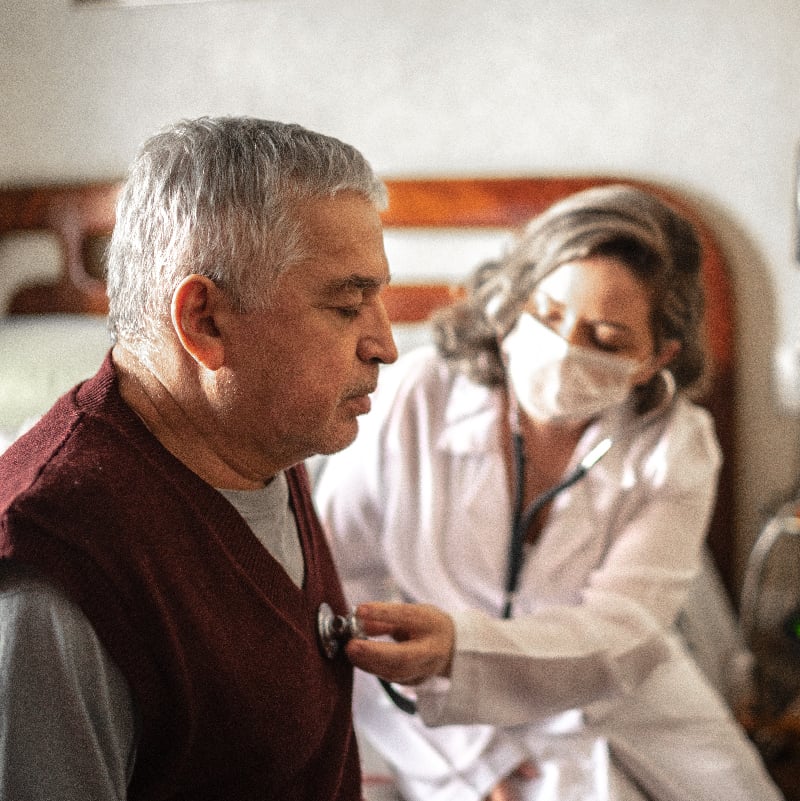
The implications of the study point to the need for clinicians to recognize and identify Black women – especially in the 20-29 age group – as being at high risk of poor cardiovascular outcomes during pregnancy.
As a result, health care providers seeing pregnant Black women patients may need to screen and monitor them more closely to ensure better health outcomes.
Adding to the complex nature of the topic is the need to account for socioeconomic variables including structural racism/bias, health literacy, and diet. The more clinicians can investigate these other variables, the better they can put a name to the factors that are impacting the health outcomes of so many people.
“Our hope is that these findings can better inform clinical practice guidelines and public health efforts,” Dr. Shamaki said. “By providing proper interventions to Black women at younger ages, provider may be able to prevent maternal mortality and improve overall health outcomes.”