Allergies are not fun, and some are harder than others to identify, diagnose, and treat. Food Protein-Induced Enterocolitis Syndrome (FPIES) and Eosinophilic Esophagitis (EoE) are two that wreak havoc and are often misdiagnosed. Never fear–Rochester Regional Health’s Allergy Program is home to expert providers at the forefront of research and treatments. We prioritize accurate diagnostics, and won’t leave a single stone unturned.
With the help of Peter Capucilli, MD, Allergy and Asthma provider at Rochester Regional Health, we discussed the differences between these two allergies, and how your allergy provider can help you.
Food Protein-Induced Enterocolitis Syndrome
What a name! FPIES (pronounced F-pies) is a rare food allergy that affects the gastrointestinal system. It is a non-IgE immune reaction, meaning that the symptoms are different than “classic” allergy, which usually involves hives, swelling and sometimes trouble breathing. FPIES is y characterized by vomiting and sometimes diarrhea. Unlike the classic food allergies, symptoms do not begin immediately after eating–instead, it can take hours for severe symptoms to show.
The most common food triggers are cow’s milk, soy, rice, and oats, but any kind of food can cause FPIES symptoms. Symptoms can lead to other complications, including lethargy, changes in blood pressure and body temperature, and failure to thrive. Upon finding and removing the problem food(s) from the diet, all FPIES symptoms subside.
Commonly, FPIES is misdiagnosed as a severe stomach illness because the symptoms are very similar. Only after repeated ingestion of the trigger food and severe symptoms hours later is FPIES typically determined as the cause.
Signs and Symptoms of FPIES
Symptoms vary child by child and in severity, and may include:
- Profuse Vomiting, usually occurring two hours after ingesting the trigger food
- Changes in body temperature and blood pressure
- Dehydration
- Diarrhea (after vomiting)
- Extreme lethargy
Dr. Capucilli explained that, “children who have chronic FPIES may have recurrent episodes of vomiting throughout the day and it can be difficult to associate timing of food exposure with symptoms. If left untreated, this condition can impact growth and your baby’s ability to thrive.”
Diagnosis and Testing
Diagnosing FPIES tends to be challenging, primarily because commonly used allergy tests like skin prick tests or blood tests do not detect this condition. It can also be difficult to recognize the food as a trigger as symptoms do not develop immediately after ingestion. Often, children with FPIES also have other food allergies, which can complicate diagnosis.
The best way to get a conclusive, accurate diagnosis of FPIES is with the help of our experienced allergists at the Rochester Regional Health Allergy Program. Their extensive research and education dedicated to complex allergies allows them to be powerful allies and provide the best possible care.
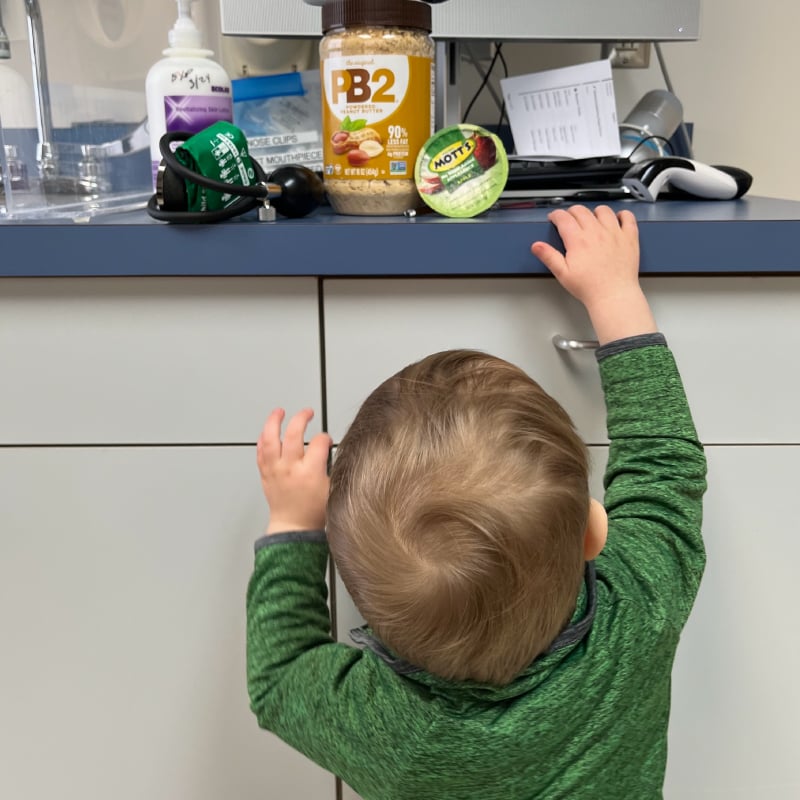
After considering your child’s medical history and symptoms, your allergist may order certain blood tests or suggest a supervised oral food challenge test. Our providers perform more than 300 oral food challenges each year, frequently utilizing the “gold standard” of diagnostic options.
Treating FPIES
Treatment for FPIES is on a case-by-case basis, since every child’s reaction is different. Dr. Capucilli added that, “the first step is recognizing and pinpointing which food(s) are your child’s problem, and then avoiding those so that your baby can feel better before we work to determine a long-term plan.”
Most children outgrow FPIES, but our team will be by your side every step of the way.
Eosinophilic Esophagitis (EoE)
Eosinophilic esophagitis (EoE) is an food-driven allergic condition that causes inflammation in your swallowing tube (your esophagus). Found at the upper part of your GI (gastrointestinal) tract, your esophagus is the tube that moves food from your mouth to your stomach when you swallow. When a large number of eosinophils, which are white blood cells, pile up and cause damage to your esophagus, we call it EoE.
Eosinophils are a special kind of white blood cells that (like other white blood cells) help fight certain types of infections, but they also play a uniquely large role in allergy and allergic conditions that may affect the body. While eosinophils are often present throughout the GI tract, they are not usually found in the esophagus. If EoE develops, large numbers of eosinophils can be found in the esophagus and can cause symptoms that alert our allergists to the problem. In addition to a careful history, our Allergy Center providers look at the number of these cells in the lining of the esophagus to help make the diagnosis.
Signs and Symptoms of EoE
Like FPIES, symptoms of EoE vary person by person. EoE symptoms also vary by age–young children may experience poor weight gain and problems eating and vomiting. Older children and adults may have chest pain, stomach pain, trouble swallowing, and reflux (heartburn). If left untreated, over time, this condition can lead to hardening and narrowing of the esophagus, which can make it difficult to swallow. Patients may even begin to have food regurgitation, feelings of food moving slowly down and food impactions, which can be an emergency.
Common symptoms include:
- Difficulty swallowing
- Pain with swallowing
- Food moving slowly down
- Failure to thrive (weight loss and poor growth)
- Food getting stuck in the throat
- Recurrent vomiting or regurgitation
- Malnutrition
- Nausea and vomiting
- Poor appetite
- Reflux that does not respond to treatment
Similar to FPIES, although EoE is typically considered a “food allergy,” symptoms do not include immediate hives, swelling or trouble breathing right after eating the food. Likewise, commonly performed skin prick tests or allergy blood tests do not diagnose EoE. Symptoms of EoE can occur days or weeks after ingesting a food allergen, and they may also come and go. This can be confusing and make accurate diagnosis difficult.
Diagnosing EoE
“A thorough history is the most important part of diagnosing EoE, however determining the number of eosinophils in the esophagus is also imperative,” explained Dr. Capucilli.
The most accurate way to diagnose is with an upper GI endoscopy, performed by one of Rochester Regional Health’s gastroenterologists. During the “scope,” the doctor will take small tissue samples and photos of the esophagus to look for eosinophils. A pathologist will review these samples under a microscope–if they find more than 15 eosinophils, then EoE is a possibility.
How do you treat EoE?
We treat EoE in two ways–dietary changes and medication. Sometimes, one or the other is enough to regulate and treat your EoE, but often a combination of both leads to strong results. Importantly, treatment for EoE does not follow a “one size fits all” approach. Your allergist will work with you to find the best course of action for your individual needs.
Since EoE is usually triggered by food, many people respond well to dietary changes and removing trigger foods from their diet. There are three dietary therapies commonly suggested for EoE: elemental diet (a liquid, formula-based diet), an empiric elimination diet (avoiding major food allergens), and a testing-directed elimination diet. Speak with your allergist regarding the benefits of these approaches.
Medications have also proven useful in treating EoE. Proton pump inhibitors can keep eosinophils from collecting in the esophagus and are safe for children as young as one year old. Corticosteroids can reduce swelling in the esophagus and make swallowing easier and less painful. Your provider will help you decide what treatment type works best for you and your family.