After ten years of fertility treatments, Jennifer and Hector were expecting their first child. Jennifer faced long-term fertility issues and multiple failed pregnancies before she was finally able to conceive. This history made the beginning of her pregnancy nerve-wracking, and required her to be induced at the end just because she made it to her due date.
The beginning of delivery
Several hours into labor, the decision was made to transition Jennifer to have a cesarean section.
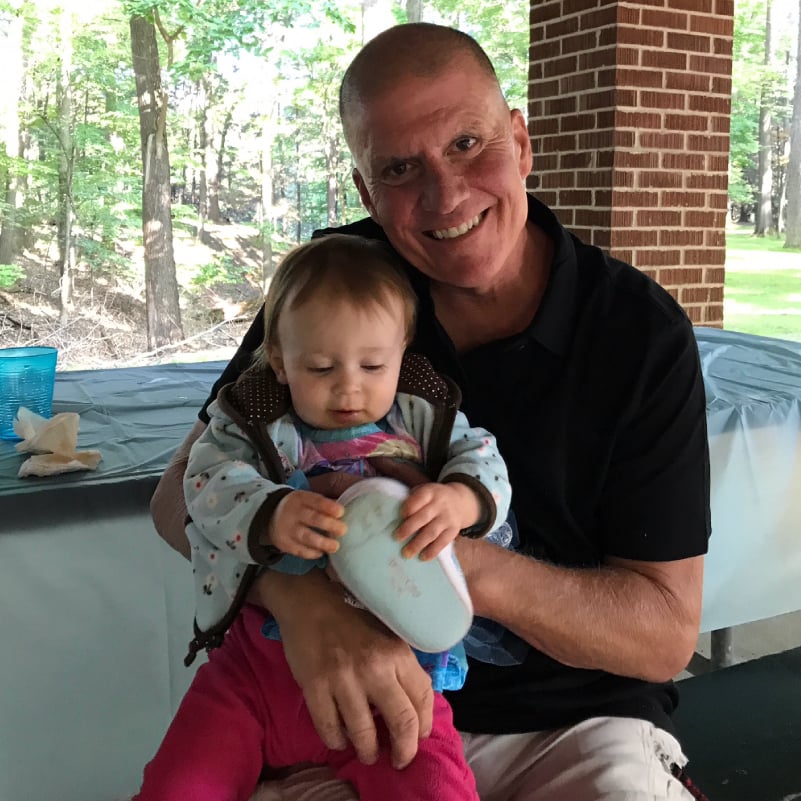
On March 9, 2018, Jennifer gave birth to Luca – a 7 ½ lb. baby boy. The surgery itself was fine, but Jennifer began having some more bleeding than usual. Her team of providers watched her for a while, and when she was stable (from a bleeding standpoint), they decided to transfer her to the surgical ICU.
Between the operating room and the surgical ICU, Jennifer started to experience several critical issues. Her lungs essentially collapsed and she could not get enough oxygen. She also started bleeding again and doctors thought they might lose her.
That is when the decision was made to do the hysterectomy and the ECMO team was called.
'Split second decisions'
“I met Jennifer under duress in a very bad situation and we had to make some split second decisions about how to proceed and what we can do to help stabilize her,” said Dr. Scott Feitell, MD, who is part of the Heart Failure & Mechanical Circulatory Support team at the Sands-Constellation Heart Institute.
“Literally as the surgeons were doing the hysterectomy, we were implanting an ECMO circuit. Basically it’s cardio pulmonary support. It provides full support for a failing heart or failing lungs. This machine gives you the chance to buy time."
“She again was hemorrhaging into her abdomen and lost multiple more units of blood, received multiple transfusion units,” Dr. Feitell continued. “Jen had to have nine surgeries and we almost lost Jen three times.”
After 12 days, Jennifer was taken off of ECMO. At that point, every day became a dramatic improvement.
“Slowly but surely she started waking up and talking to us. It was just fantastic,” Dr. Feitell said.
“You know, I was given a second chance at life for some reason,” Jennifer said. “I’m very lucky for it and it was a miracle that I had him after everything that I went through and it was wonderful. It was amazing. I was home and I had my baby and my family. It was more than I could ever hope for.”
Coming together to save a life
Jennifer's team believes the collaboration of care between multiple departments in this hospital were paramount to her survival.
“There are certain moments in your medical careers that you’ll never forget and this is probably one of those cases that I’ll never forget,” Dr. Feitell said. “We are very fortunate to have ECMO at Rochester Regional Health. It’s still considered cutting edge technology and there are many systems in many hospitals around the world that don’t have access to it. As our system as a whole expands into more regions in upstate New York, there are sick patients out there and there’s a lot of hospitals that simply don’t have the resources to run this program. By having these machines available, it allows us to take patients that are very sick from all throughout New York state and again stabilize them and hopefully fix them, hopefully get them better and have them walk out of the hospital like Jennifer did.”
“It’s amazing how all the teams came together for me and pulled for me and pulled for Luca to bring us back together and get us home,” Jennifer said. “That’s what they did. And because of them, my son will still have a mom.”
“Thank you for saving my life and being there for my family. Just thank you. I can’t say that enough. I can’t do enough for them to let them know how much I appreciate them. It’s just…thank you for everything you guys do.”