Dying is a natural part of life. As a patient’s life comes to an end, providers with hospice care teams work together to ensure patients are comfortable during the last days and weeks of the patient’s life, no matter where they are.
Hospice care focuses on comfort, limiting medical interventions, and allowing a person to die naturally – whether at home, in a hospital, or an in-patient facility.
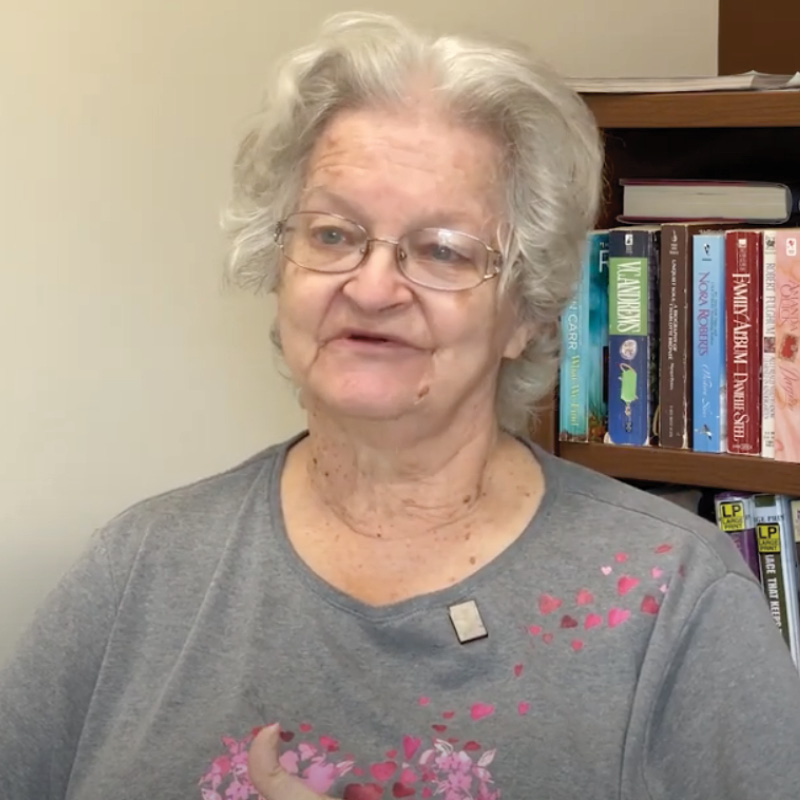
We talked with Nina Cain, a Rochester Regional Health Hospice Care team manager, and Farress Crombe, RN, a hospice care nurse at the Elizabeth G. and Jennifer J. Hildebrandt Hospice Care Center, and asked them to share some of their experiences.
What hospice patients say
There are some misconceptions when it comes to hospice care and dying, in part based on popular culture and a lack of talking openly about death.
In Cain’s experience while caring for dying patients, dynamics and communication styles are different for each family. No two families are the same, so no one goes through the same experience. But there are some common feelings that are shared.
“Oftentimes, patients and their families want to reminisce,” Cain said. “They find a lot of joy and comfort in that and reliving those old stories of what their life was like before they were sick.”
At the same time, there is a desire for patients to know their families are present and will support any hospice-related choices in the days leading up to their death.
“Ultimately, patients want to know that they're loved,” Cain added. “I think, one of the biggest things that families can communicate is that a patient is loved, that they're there to support them, and give them permission to let go.”
While working at the Hildebrandt Hospice Care Center, Crombe said patients who are on hospice care almost never express fear of death. Hospice patients are usually at peace or accepting of death.
What hospice patients are fearful of, Crombe said, is being a burden to their family, being abandoned or forgotten, dying alone, or having uncontrollable pain in their last days. The role of hospice care staff is to ease those worries.
Hospice care teams
Each hospice care team is interdisciplinary, bringing together different areas of health care expertise to provide comfort measures for patients who need end-of-life care.
The core of the team are the nurse and social worker. These two are the ones who primarily provide care and support to the patient and their family. Other team members include spiritual care staff, bereavement support staff, home health aides, volunteer services, a medical director, as well as the patient's primary care doctor.
Together with the patient and their family, a hospice care team collaborates to provide the desired care through medications, counselors, spiritual care, and other measures.
“Although what we do is sad and it can be heavy at times, we find a lot of joy in being the ones to provide care for, and support patients and families at end of life,” Cain said. “It can be very rewarding, especially at a time when patients and families are at their most vulnerable. We're able to be there and support them and guide them through a difficult time.”
Being prepared
As difficult as talking about death can be, knowing there is a plan in place for end of life can take a lot of the burden of complex medical decision-making off the shoulders of a person and their loved ones – especially if someone is unable to communicate their wishes.
Creating a Medical Order for Life-Sustaining Treatment (MOLST) is designed for seriously ill patients with advanced medical conditions in order to provide a high quality of care at the end of life. This document is filled out by health care professionals and clearly outlines life-sustaining treatments that a patient currently wants to receive or avoid.
An advanced care directive, such as a living will or health care proxy, are filled out by patients themselves and document a patient’s preferences for future care. These directives can be filled out by any person age 18 or older.
When the time comes, a patient or their loved one can reach out to the patient’s physician and request a referral for hospice care. A member of the hospice care team will set up a time to meet the patient and their family to perform an evaluation, which explains the program to ensure it’s a good fit for everyone and that patient meets hospice criteria based on Medicare guidelines.
“Having this information in advance before it's needed is so important,” Cain said. “With these measures in place, families and patients can be prepared and really express what their wishes are at end of life.”